Birth control pills
Birth control pills may block, delay or cause ovulation. “Ovarian suppression” in birth control pills primed ccyles may have an alternative explanation.
The idea behind birth control pills is very simplistic: during the pregnancy woman’s serum progesterone is high and her periods stop, it stood to reason that giving progesterone to a woman who is not pregnant will also stop her period.
Natural progesterone has poor oral absorption and a very short half-life to be useful for a sustainable increase in blood. Therefore, it could not be used for birth control. Then micronized progesterone, with a much better oral absorption was developed, but its half-life was still too short. Finally, synthetic compounds exhibiting progesterone activity – progestins, with excellent oral absorption characteristics as well as a long half-life, came to the market.
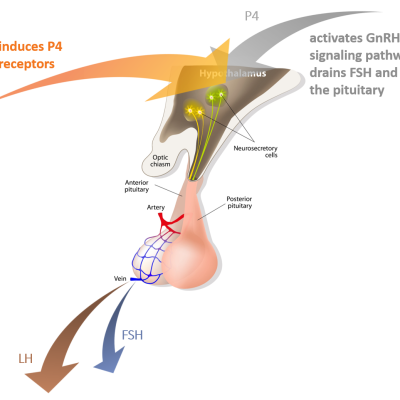
There are many brands of birth control pills with different amounts and kinds of progestins. Progestins mimic the action of progesterone, which is according to our theory is a natural, the most upstream trigger of gonadotropins surge. It activates GnRH signaling pathway by binding to its receptors in the hypothalamus. The number of progesterone receptors is upregulated by estradiol. This explains why birth control pills have to be started at the beginning of the cycle: if the first pill is taken in the middle of the cycle the pill may actually cause ovulation.
It is very important to appreciate that birth control pills cannot be compared by the amount of progestin they contain. This is because their relative progesterone-like activity varies vastly. For example, dydrogesterone is 20 times more potent than natural progesterone, while D/L norgestrel is about 3,000 times more potent than progesterone.
Unfortunately, the relative activity for many modern progestins is not publicly available. As a side note, according to our theory, the high level of progesterone during pregnancy desensitizes its own hypothalamic receptors and therefore it may take several months after delivery to resume ovulation. Because the activity of progestins in the pills is similar to the progesterone during pregnancy (maybe even higher), it may also take several cycles before ovulations resume. More about progesterone
The number of progesterone receptors and progesterone act synergetically. Adding estradiol into the birth control pill increases the number of progesterone receptors, thereby reducing the progestin activity required to lower the level of gonadotropins in circulation. On the other hand, progestin-only pills generally need higher progesterone-like activity to be effective.
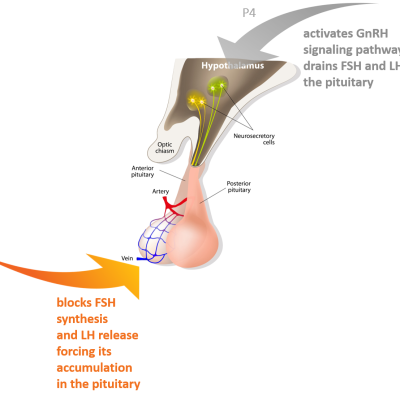
In addition to inducing progesterone receptors, estradiol also suppresses the synthesis of FSH and the release (but not synthesis!) of LH from the anterior pituitary.
Thus, E2 and P4 have synergism at the upstream of a GnRH signaling pathway and relative antagonism at the level of pituitary. The antagonism is relative because, without E2, gonadotropins accumulation and therefore their massive release by P4 would not be possible. Yet, the progesterone-induced release of gonadotropins always trumps the blocking action of E2. Figuratively speaking, E2 serves as a plug at the bottom of the barrel, that allows accumulation of the fluid so that it can be emptied at once creating a surge by rising P4.
Curiously, in theory, estradiol alone could also be used to prevent ovulation. However, in practice, this is not possible, because: 1. the high level of E2 required for effective suppression of gonadotropins has serious side effects and 2. accumulated LH would be breaking through from time to time.
Birth control pills in ovarian stimulation protocols
Birth control pills greatly simplify the management of an ovarian stimulation protocol and embryo transfers and in some cases allow a more uniform growth of the follicles. They enable the creation of what appeared as an ovarian cycle in which the first day is completely controlled. In a typical protocol, a patient will take birth control pills for several weeks or longer. When ready to start the stimulation, birth control pills are canceled. The bleeding that follows is used as a benchmark of a new follicular cycle.
Sometimes it is observed that after priming with birth control pills there are fewer follicles recruited into the cycle than expected. This phenomenon, known as “ovarian suppression”, is attributed to estradiol and progesterone indirect action, upstream of the hypothalamic-ovarian axis. However, according to the current paradigm follicles’ recruitment into the follicular phase is hormone-independent, ovarian suppression remains enigmatic.
There is evidence that in reality, follicular recruitment is not completely hormone-independent. Instead, observations suggest that rising FSH superimposes on the recruitment process creating an increase in follicles recruitment when it rises two times during the cycle: at the time of gonadotropins surge before ovulation and at the end of the luteal phase. Even though progestins and estradiol present in birth control pills lower gonadotropins (LH and FSH) levels in circulation, there is strong evidence that in most cases this suppression is only partial so that FSH continues to fluctuate creating nonrandom waives of follicles recruitment. As the result, when birth control pills are stopped at a random and gonadotropin stimulation started, the artificial cycle will sometimes ride a pre-existing waive of the follicular recruitment, creating a normal response and sometimes will not, creating an appearance of suppression.
Therefore, many physicians evaluate the status of the follicles in the ovaries before stopping the pills to confirm that the timing to start ovarian stimulation relative to the possible spontaneous wave of the follicles is optimal.